

Rightway connects your employees to high-quality, cost-effective care through our healthcare navigation platform. Our clinical care guides handle everything from appointment scheduling to benefit navigation, reducing your team’s workload while improving outcomes.
Employees connect with a dedicated health guide by app or phone. Our clinical care navigation team answers questions, coordinates appointments, and handles administrative tasks so your team doesn’t have to.
Rightway’s clinical health advocates uncover needs early and guide members to high-value care. This patient care navigation model improves outcomes while lowering employer healthcare costs.
Rightway guides members to high-value care and proactively supports high-risk members to drive healthcare value. A 2:1 ROI guarantee ensures that your team gets results.




Employees connect with their health guide through our intuitive app, accessing clinical navigation, benefit support, and personalized care recommendations in one place. Or they can reach us by phone - whatever works best for your team.
Our health guides answer employee questions, manage healthcare logistics, and direct members to high-value care. Each team is led by experienced clinicians including nurse practitioners and registered nurses, ensuring every recommendation is grounded in medical expertise.
Rightway’s proprietary Advocate Platform analyzes 10,000+ data points to identify risks, trigger alerts, and enable proactive care navigation. Our health guides use these insights to engage members early, close care gaps, and deliver tailored support at scale.
Our analytics platform tracks ROI, member engagement, and navigation-driven cost savings in real time. Your dedicated Customer Success Manager delivers quarterly reports and partners with you to optimize strategy, performance, and outcomes.
The Advocate Platform evaluates provider quality using proprietary and third-party data. Clinical guides then match members with top-performing providers to improve care outcomes and reduce unnecessary costs.

Our platform analyzes 10,000+ data points to surface high-risk and rising-risk individuals. These insights power timely clinical outreach, personalized navigation, and targeted engagement that improve health outcomes and lower spend.
Members get fast, virtual access to licensed clinicians—right from our navigation platform. Telemedicine ensures convenient, cost-effective care while keeping health guides involved in every decision.
Rightway care navigation combines expert advocacy, clinical guidance, and personalized support to drive measurable healthcare value. Your employees make smarter decisions, while you reduce costs and save time.
Schedule a demo
Reduction in total healthcare costs
Average employee engagement
Average ROI on employer healthcare spend
Member Net Promoter Score
Rightway serves as your employees’ entry point to smarter healthcare decisions. Our health guides connect members with high-value care and services, helping benefits teams achieve better engagement, outcomes, and ROI.
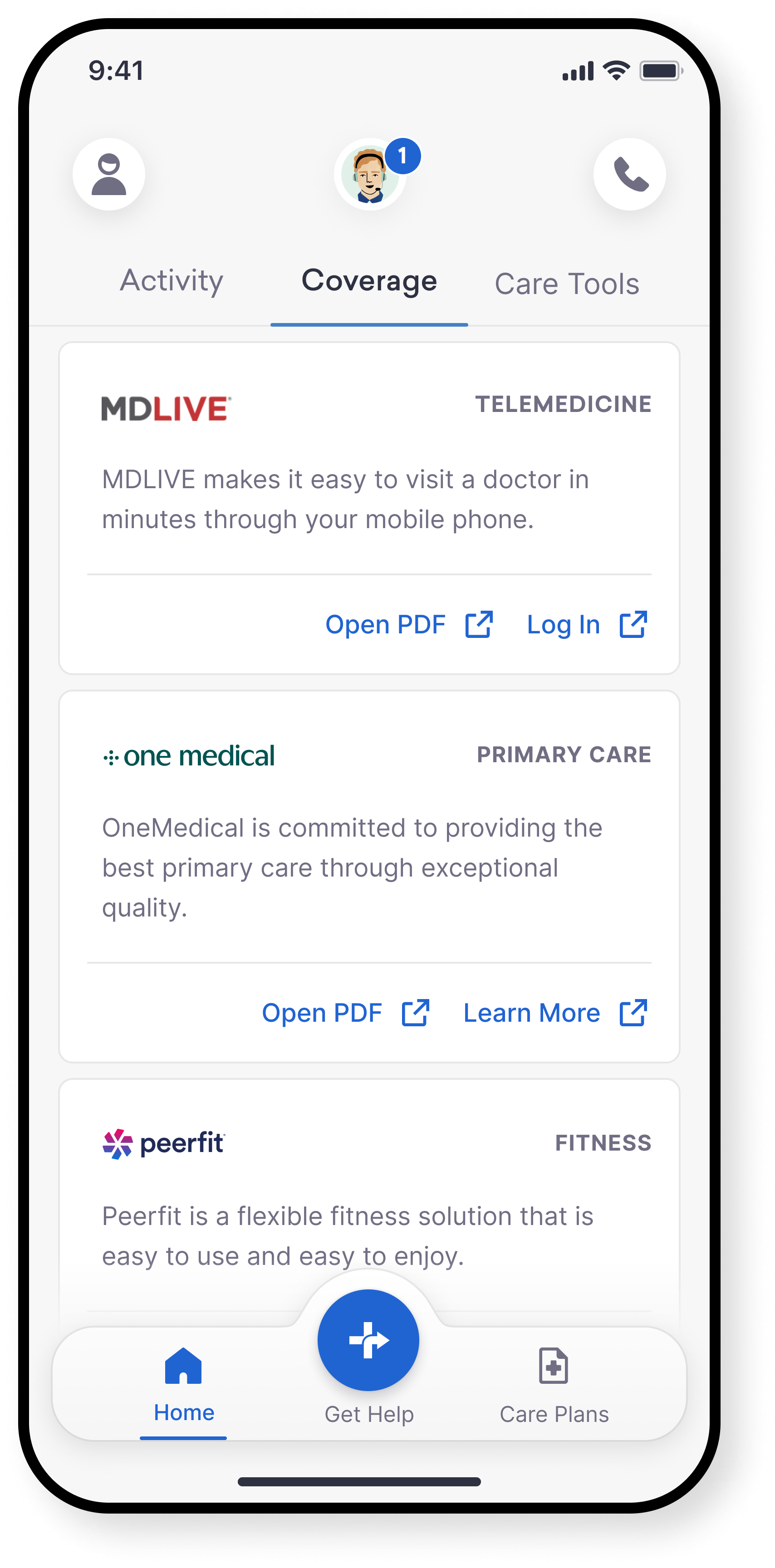
Give your employees 24/7 access to licensed clinicians, anytime, anywhere. From everyday symptoms to behavioral health needs, members get fast, cost-effective virtual care that reduces reliance on high-cost ER and urgent care visits.

“Rightway helped us reduce our total healthcare spend by 5% and non-catastrophic spend by 9%, while engaging 62% of our employees in the first year.”
Short on time? Rightway can save you 12 hours a week.
See how care navigation gives you time back.